Prostatitis is a condition that refers to the inflammation of the prostate gland, a small walnut-shaped organ located just below the bladder in men. The prostate plays a crucial role in producing seminal fluid, which nourishes and transports sperm. When this gland becomes inflamed, it can cause various symptoms, including pain, difficulty urinating, and sexual problems. Prostatitis can be acute or chronic, and it may result from an infection or other factors that irritate the prostate. In this blog, we will explore the causes, symptoms, diagnosis, and treatment of prostatitis to help you understand this common condition better.
What is Prostatitis?
Prostatitis is the inflammation of the prostate gland, often resulting in pain and discomfort. It is one of the most common urological problems in men, especially those aged between 30 and 50. There are several types of prostatitis, including acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis.
Causes of Prostatitis
The causes of prostatitis can vary depending on the type of prostatitis. Here are some of the key causes:
- Bacterial Infection:
- Acute Bacterial Prostatitis: This is a serious infection caused by bacteria, often from urinary tract infections (UTIs) or sexually transmitted infections (STIs) like chlamydia or gonorrhea. It can also be caused by infections that spread from other parts of the body to the prostate.
- Chronic Bacterial Prostatitis: This is a less common form of prostatitis but involves a long-term bacterial infection of the prostate, typically caused by the same bacteria as acute prostatitis.
- Chronic Pelvic Pain Syndrome (CP/CPPS): CP/CPPS is a condition in which the prostate becomes inflamed, but no bacterial infection is present. The exact cause of CP/CPPS is not well understood, but it may be linked to nerve irritation, muscle tension in the pelvic area, or stress.
- Urinary Tract Infections (UTIs): Repeated UTIs can lead to bacterial prostatitis as bacteria travel from the urinary tract into the prostate.
- Bladder or Urinary Tract Obstruction: An obstruction in the urinary tract or bladder can create conditions where bacteria are more likely to accumulate and cause an infection, leading to prostatitis.
- Pelvic Trauma: Injuries or trauma to the pelvic area can result in inflammation of the prostate. This may occur after surgery or physical injury.
- Sexually Transmitted Infections (STIs): Certain STIs, like chlamydia and gonorrhea, can cause prostatitis, particularly in sexually active young men.
- Autoimmune Disorders: In some cases, the body’s immune system may mistakenly attack the prostate tissue, causing inflammation. This can contribute to the development of prostatitis.
Symptoms of Prostatitis
The symptoms of prostatitis can range from mild to severe, and they vary depending on the type of prostatitis. Common symptoms include:
- Painful Urination: One of the hallmark symptoms of prostatitis is dysuria (painful urination). The pain may be sharp or burning and is usually felt during or after urination.
- Frequent Urination: Men with prostatitis often experience a frequent urge to urinate, especially at night (nocturia). This can be due to irritation or pressure from the inflamed prostate.
- Painful Ejaculation: Prostatitis can cause pain during or after ejaculation, affecting sexual function and causing discomfort.
- Pelvic or Lower Abdominal Pain: Pain or tenderness in the pelvic region, lower abdomen, or lower back is common. This pain may be constant or may come and go.
- Flu-like Symptoms: In cases of acute bacterial prostatitis, the infection can lead to fever, chills, and fatigue. It may also cause nausea and vomiting.
- Blood in Urine or Semen: Some men with prostatitis may notice blood in their urine or semen, a condition known as hematuria.
- Erectile Dysfunction (ED): Prostatitis, especially chronic pelvic pain syndrome (CP/CPPS), can cause sexual difficulties, including erectile dysfunction.
Diagnosis of Prostatitis
Diagnosing prostatitis typically involves a combination of medical history, physical examination, and diagnostic tests. Here’s how it is generally diagnosed:
- Medical History and Symptoms: A doctor will begin by asking the patient about their symptoms, including any pain, urinary issues, or sexual problems. The doctor will also inquire about any past history of infections, surgeries, or injuries.
- Digital Rectal Exam (DRE): The doctor may perform a digital rectal exam (DRE), where a gloved finger is inserted into the rectum to feel the size and tenderness of the prostate gland. This helps the doctor assess any swelling or abnormal texture in the prostate.
- Urine Tests: A urine sample may be taken to check for signs of infection, such as bacteria or blood. Urinalysis helps diagnose bacterial prostatitis and rule out other conditions like a urinary tract infection (UTI).
- Blood Tests: Blood tests may be conducted to check for signs of infection or inflammation. Elevated white blood cell counts may indicate an infection.
- Prostate Fluid Cultures: If bacterial prostatitis is suspected, the doctor may take a sample of the prostate fluid (obtained through a prostate massage during the rectal exam) to test for bacterial infection.
- Transrectal Ultrasound (TRUS): A transrectal ultrasound can be used to examine the prostate gland. This test uses sound waves to create images of the prostate and can help identify any structural abnormalities.
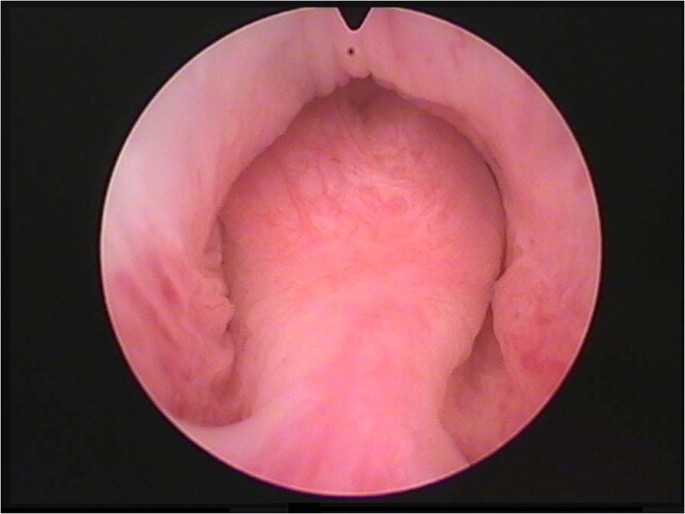
- Cystoscopy: In some cases, a cystoscopy, which involves inserting a small camera into the bladder, may be performed to assess the urinary tract and look for signs of obstruction or infection.
Treatment of Prostatitis
Treatment for prostatitis depends on the type and severity of the condition. The main goal of treatment is to relieve symptoms and treat the underlying cause with consultation of best urologists. Here are the most common treatment options:
- Antibiotics:
- Acute Bacterial Prostatitis: This condition is usually treated with a course of oral or intravenous antibiotics. In some cases, hospitalization may be required if the infection is severe.
- Chronic Bacterial Prostatitis: Long-term antibiotic therapy may be necessary to clear the infection. Treatment can take several weeks or even months.
- Alpha-Blockers: Alpha-blockers, such as tamsulosin, help relax the muscles of the prostate and bladder neck, making it easier to urinate and reducing symptoms of prostatitis.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs like ibuprofen can help reduce inflammation, pain, and fever associated with prostatitis. They provide relief from pain and swelling in the prostate.
- Prostate Massage: Prostate massage may be performed by a healthcare provider to help relieve symptoms, particularly in cases of chronic pelvic pain syndrome (CP/CPPS). This procedure helps stimulate the prostate and can promote drainage of fluid buildup.
- Physical Therapy: Pelvic floor physical therapy may be recommended for chronic prostatitis to help relax tight pelvic muscles, reduce pain, and improve pelvic health.
- Surgery: Surgery is typically a last resort for men with severe or chronic prostatitis that does not respond to other treatments. Surgical options may include drainage of an abscess or removal of prostate tissue.
- Lifestyle Changes:
- Dietary Modifications: Avoiding spicy foods, caffeine, alcohol, and acidic foods may help reduce inflammation and alleviate symptoms.
- Stress Management: Reducing stress through relaxation techniques, yoga, or mindfulness can help manage CP/CPPS symptoms.
- Heat Therapy: Applying heat to the pelvic area, such as with warm baths or heating pads, can provide relief from pain and inflammation.
Conclusion
Prostatitis is a common condition that can significantly affect a man’s health and quality of life. Whether it’s caused by bacterial infection or pelvic pain syndrome, prostatitis can lead to symptoms such as pain, difficulty urinating, and sexual dysfunction. However, with proper treatment, most men can manage their symptoms and lead a healthy life. If you experience symptoms of prostatitis, it’s important to consult a healthcare provider to get an accurate diagnosis and appropriate treatment. Early intervention can help prevent complications and improve overall health.
FAQs
- What causes prostatitis? Prostatitis can be caused by bacterial infections, urinary tract infections (UTIs), trauma to the pelvic region, sexually transmitted infections (STIs), or autoimmune conditions. Chronic pelvic pain syndrome (CP/CPPS) is another cause, though its exact cause remains unclear.
- How is prostatitis diagnosed? Diagnosis involves a physical examination (including a digital rectal exam), urine tests, blood tests, and sometimes prostate fluid cultures or imaging tests like a transrectal ultrasound. The type of prostatitis determines the specific diagnostic approach.
- What are the treatment options for prostatitis? Treatment for prostatitis may include antibiotics for bacterial infections, alpha-blockers to relieve urinary symptoms, NSAIDs for pain relief, pelvic floor physical therapy, prostate massage, or in severe cases, surgery. Lifestyle changes, including stress management and dietary modifications, can also help alleviate symptoms.